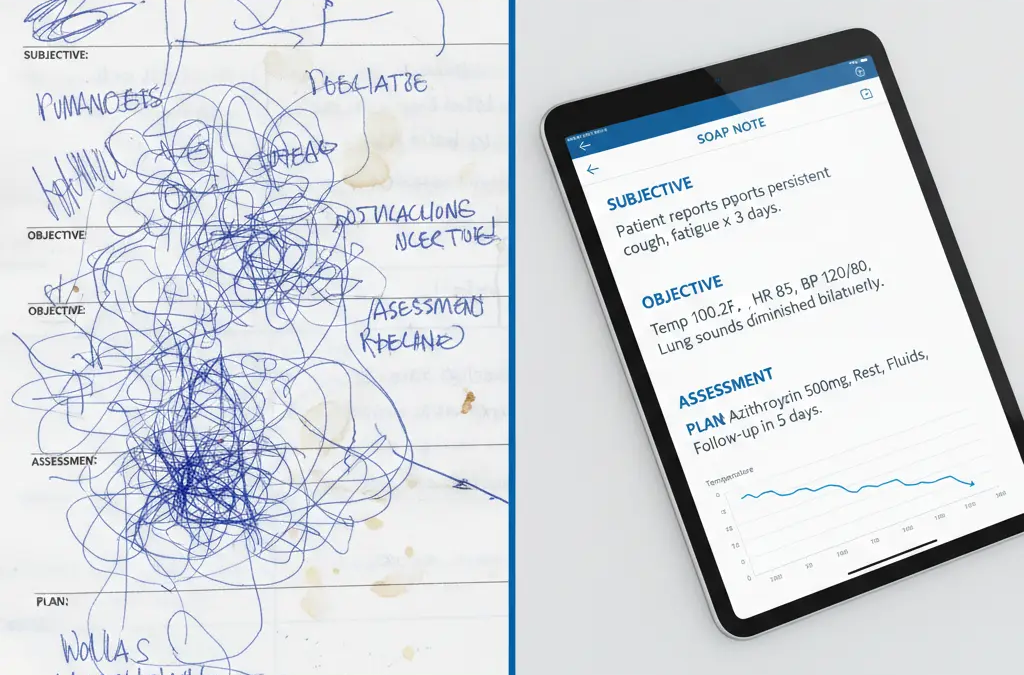
You have heard a million times, in the field of healthcare, that, unless recorded, it did not occur.
However, what they leave out is the following: bad documentation does not simply imply that it did not take place, it only that you will not get paid, and that you will have to fill out charts way after everybody else has left.
To doctors who are buried in paperwork and the virtual scribes that are on their learning curve, the SOAP note is not a form to fill in. It is the difference between coming out of the office in 5 PM or midnight.
The good news? It is all different when one masters the SOAP note format.
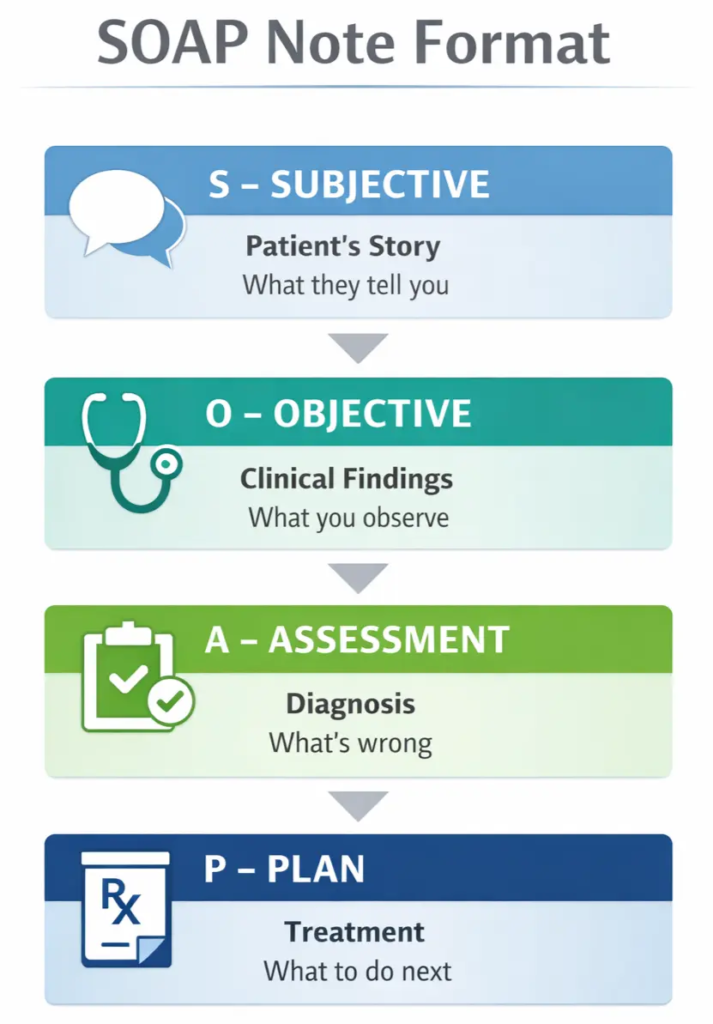
What is a SOAP Note?
SOAP is an acronym that means Subjective, Objective, Assessment and Plan.
It is the gold standard in medical records as it makes the patient information arranged in a logical manner. The chart can be picked up by any provider, and he or she can know what is wrong, what was discovered and what to do immediately.
Consider it as a medical detective:
- The eyewitness (Subjective) testimony.
- The objective evidence (Personal Statement)
- The deduction (Assessment)
- The next steps (Plan)
The 4 Parts of a SOAP Note
Subjective: what the Patient Says.
This is the self account of the patient. What brings them in today?
Important factors: Chief complaint, when it began, severity of it, what aggravates or relieves it.
Example: “Patient complains of sore throat which began 3 days ago. Pain 4 /10, exacerbates upon swallowing.
Subjective: What the Doctor Sees.
Pure facts. Numbers. Measurements. Observations. No opinions.
Significant aspects: Vital signs, physical examination, laboratory data.
Sample: “T 99.1 deg F, red and swollen throat, lungs clear.
Evaluation: What is the Diagnosis?
The doctor connects the dots. On what the patient reported and what was discovered, what is happening?
Location Upper respiratory infection (probably viral).
Plan: What’s Next?
The action steps. Medications, examinations, referrals, and follow-up.
Ex: rest, liquids, pain medication (Tylenol). Return if fever exceeds 101degF.”
SOAP note, 5 examples in the real world.
Supply: The supply is the BP monitor together with the 24 hour BP device (BPVM).<|human|>Demand: The demand is the BP monitor and the 24 hour BP device (BPVM).
Subjective:
Here to have blood pressure checked and to refill medication. Taking Lisinopril 10mg daily. Denies any chest pain, dizziness, and headaches. Walking 30 minutes daily. Home blood pressure is 130 /85.
Objective:
BP 128/82, HR 72. Normal cardiac rhythm, diaphragm clear, no edema in legs.
Assessment:
Hypertension, already under medication.
Plan:
Carry on with Lisinopril 10mg daily, low-salt diet, walks. Order cholesterol test. Return in 6 months.
Background: A 52-year-old male patient diagnosed with a sore throat and cough one month ago.
Subjective:
Sore throat started 3 days ago. Throat feels scratchy (4/10 pain). Dry cough with congestion. No fever. Roommate is sick too. DayQuil helped a little.
Objective:
Temperature 99.1degF, BP 118/76. Throat erythema not extensive, no white spots. Neck has slightly swollen lymph nodes. Lungs clear.
Assessment:
Viral or common cold Upper respiratory infection.
Plan:
Rest and fluids. Gargle with warm salt water. Tylenol or Motrin for pain. Honey or lozenges for cough. Repeat in case the fever is above 101degF or takes a period of more than 7 days.
Example 3: Back Pain
Subjective:
The pain in the lower back began 2 days ago following the exercise of lifting heavy boxes. Pain rate 7/10 achy tight, radiates to right buttock. Aleve doesn’t help much. No bladder or bowel issues.
Objective:
Rub the spine muscles lower back. Limited bending due to pain. Normal sensation and strength of legs. Limping slightly.
Assessment:
Strain on acute lower back muscles due to heavy lifting.
Plan:
7 days muscle relaxer prescribed at bedtime. Physical therapy referral. Heat or ice therapy. None lifted more than 10 pounds in 2 weeks.
Example 4: Anxiety Follow-Up
Subjective:
Being overwhelmed about job situation. Difficulty sleeping, night worrying. Taking Zoloft 50mg. Says it helps but not enough. No thoughts of self-harm.
Objective:
Neatly clad, submissive yet restless. Speech normal. Mood anxious. Having the ability to think clearly and organically.
Assessment:
Generalized anxiety disorder, which is partially under control, heightened work stress.
Plan:
Increase Zoloft to 75mg daily. Sleep hygiene (no phone before bed). Therapy referral. Crisis hotline provided. Return in 4 weeks.

The case under consideration is the telehealth Skin Rash.
Subjective:
Red, raw circle on left forearm 4 days. Has been gardening. Fancies it is a bite of a bug or the ringworm. Hydrocortisone cream was not effective.
Objective:
Patient agreed to video examination. Video Forearm 3cm round lesion. Scalp boiled, raised, red and scaly.
Assessment:
Ringworm (dermatological infection).
Plan:
Twice a day of 2 weeks of antifungal cream. Wash hands after touching. Wash bedsheets in hot water. Re-do in 2 weeks when there is no progress.
The Benefits of Virtual Scribes to SOAP Notes.
This is the truth of the matter, writing correct SOAP notes takes a lot of concentration.
The doctors miss a thing when they are meant to listen and type simultaneously. Significant information is lost in the cracks.
The game is altered by virtual scribes.
With a skilled scribe, documentation is done in real-time and enables providers to:
- Eye contact – 10x more trustful than looking at the screen.
- Note down important information – Capture what is not there (very important in billing)
- Finish sooner – Notes are 90 percent completed by the time the patient is gone.
- Get home on schedule – No more midnight shifts
Common Mistakes to Avoid
Confusion of Subjective and Objective.
Inaccurate: “Patient at the pain level does not look good.
Right: “Guarding abdomen, patient grimacing”
The Neglect of Relevant Negatives.
Always write down what ISN’T: “Denies chest pain, no fever.
Vague Assessments
Wrong: “Patient has back pain”
Right: “Heavy lifting acute lumbar muscle strain”
Subjective (story of the patient), Objective (tests of the examination), Assessment (diagnosis), and Plan (treatment steps).
Yes, scribes compose there notes on the fly. The licensed provider is required to check it and authorize it.
To the extent that it is needed to be comprehensive. Similar visits require 1-2 paragraphs per section. Complex cases may be longer.
The Bottom Line
Medical documentation is based on the SOAP note. Get used to this format, and you will have clear and accurate records to safeguard the patients and providers.
To scribes: The fact that you can generate clean SOAP notes is of what is most valuable to you.
To the providers: Hiring someone to do your documentation is like getting back your time. No more charts at midnight.
Ready to Reclaim Your Time?
If you’re spending more time on charts than with patients, it’s time for a change.
ScribeRunner’s virtual scribes handle the documentation so you can focus on patient care.
- Cut documentation time in half
- Go home on time
- Maintain eye contact with patients
- Reduce burnout
Contact ScribeRunner:
- Phone: (786) 866-7849
- Address: 25 SE 2nd Ave, Suite 1030, Miami, FL 33131
- Hours: Monday through Friday, 8 AM to 6 PM EST
- Service Area: Miami, Fort Lauderdale, Tampa, Orlando, and nationwide
Schedule a free consultation to discuss how virtual patient care services can enhance your practice’s patient experience and operational efficiency.